Melanoma affects thousands of Americans each year and raises important questions about risk factors and prevention. While sun exposure is widely recognized as a significant contributor to melanoma development, many patients wonder about the role genetics plays in their skin cancer risk. Keep reading to learn how the genetic components of melanoma can help identify those at higher risk and emphasize the importance of appropriate screening and prevention strategies.
What Is Melanoma?
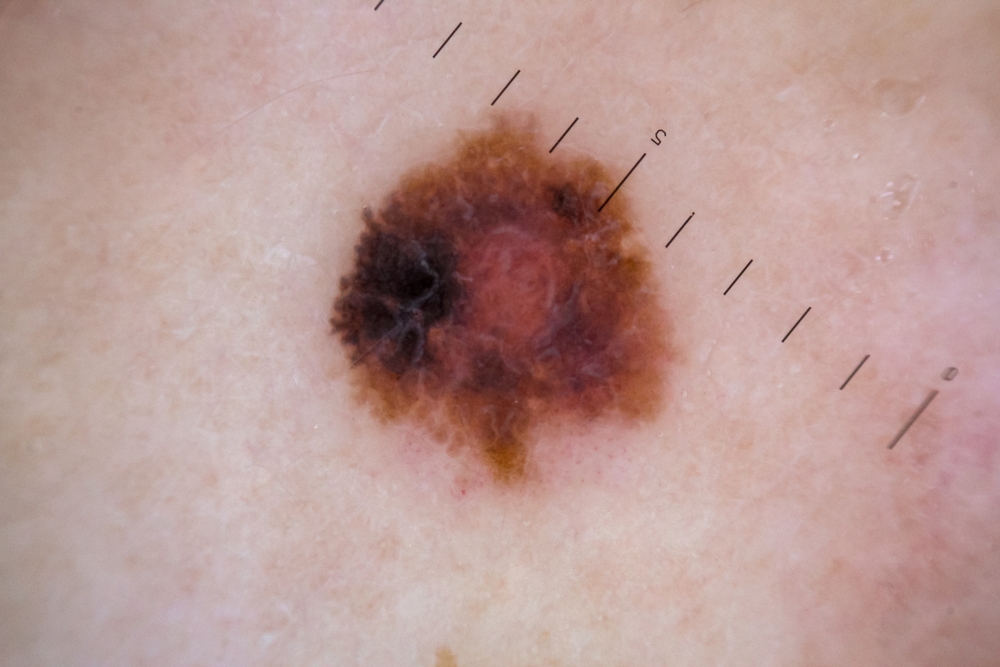
Melanoma is a type of skin cancer that develops from the cells that give skin its color, called melanocytes. Unlike more common skin cancers, melanoma can spread rapidly to other parts of the body if not detected and treated early.
Although melanoma accounts for a small percentage of skin cancer cases, it’s responsible for the majority of skin cancer deaths due to its aggressive nature. The cancer typically appears as an unusual mole or pigmented area on the skin, with characteristics that can be remembered using the ABCDE rule: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolution or change over time.
The Genetic Link to Melanoma
Melanoma can have genetic components, with family history being an important risk factor for developing this serious skin cancer. Approximately 10% of melanoma cases occur in people who have a family member with the disease.
Research has identified several specific genes associated with inherited melanoma risk. Gregory Bricca, MD, a board-certified dermatologist and Mohs surgeon at Golden State Dermatology in Roseville, explains the importance of understanding genetic risk:
“When we talk about melanoma’s genetic component, we’re looking at multiple factors that can influence risk. Some patients inherit specific gene mutations that significantly increase their susceptibility, while others may have inherited traits like fair skin and light eyes that make them more vulnerable to UV damage. Understanding these genetic factors helps us create more personalized screening schedules and prevention plans, potentially catching melanomas at their earliest and most treatable stages. This knowledge allows us to be more proactive rather than reactive in our approach to patient care.”
Inherited Traits That Increase Melanoma Risk
Beyond specific gene mutations, certain inherited physical traits are associated with higher melanoma risk. Fair skin that burns easily and rarely tans is an inherited characteristic that increases susceptibility to UV damage.
Having naturally blond or red hair, light-colored eyes, and numerous freckles or moles are also inherited traits that correlate with increased melanoma risk. These traits are often seen together in what dermatologists refer to as Fitzpatrick skin type I or II.
People with these inherited characteristics should be particularly vigilant about sun protection and regular skin checks. The genetic factors that contribute to these traits often overlap with those that influence melanoma risk.
Family History and Melanoma Risk Assessment
Having a first-degree relative (parent, sibling, or child) with melanoma approximately doubles a person’s risk of developing the disease. This risk increases further when multiple family members have been diagnosed with melanoma.
The pattern of melanoma in families can provide important clues about potential genetic causes. Early age of onset, multiple primary melanomas in one individual, and unusual melanoma locations (such as areas with minimal sun exposure) all suggest a stronger genetic component.
Alexandra Vaughn, MD, at Golden State Dermatology, highlights the importance of comprehensive risk assessment:
“Family history remains one of our most valuable tools in melanoma risk assessment, often revealing patterns that prompt more thorough evaluation. When we identify patients with significant family history, we can implement enhanced surveillance protocols including more frequent examinations and sometimes advanced imaging techniques. We also consider the possibility of genetic testing in certain high-risk families, which can guide not only the patient’s care but also risk assessment for their relatives. This multi-generational approach to melanoma prevention represents the cutting edge of precision dermatology.”
Can You Prevent Melanoma if You Have a Genetic Risk?

For those with genetic risk factors, prevention strategies should be particularly rigorous. Daily use of broad-spectrum sunscreen with SPF 30 or higher is essential, even on cloudy days.
Protective clothing, including wide-brimmed hats, long sleeves, and UV-blocking sunglasses, provides an additional layer of protection. Seeking shade, especially during peak sun hours (10 am to 4 pm), further reduces UV exposure.
Regular self-examinations and professional skin checks are crucial for early detection. Those with genetic risk factors may need more frequent professional examinations, sometimes as often as every 3-6 months.
Schedule Your Skin Cancer Screening
Melanoma has both genetic and environmental components, with several specific genes and inherited traits increasing risk. While you cannot change your genetic makeup, understanding your personal risk factors allows for tailored prevention and early detection strategies.
Regular skin examinations by a qualified dermatologist remain the cornerstone of melanoma management for those with genetic risk factors. Early detection dramatically improves treatment outcomes, even for those with genetic predispositions.
If you have questions about your skin, schedule an appointment at The Menkes Clinic today!